COBRA
Administration
From implementation to reporting, we've got your COBRA and Direct Billing needs covered.
COBRA
Administration
From implementation to reporting, we've got your COBRA and Direct Billing needs covered.
COBRA & Direct Billing Package Includes:
Implementation & Compliance
Notifications & COBRA Event Communications
Premium Collection & Remittance
Termination/End of COBRA
Renewal Processing
Employer, Broker & Participant Portals
Participant Mobile App
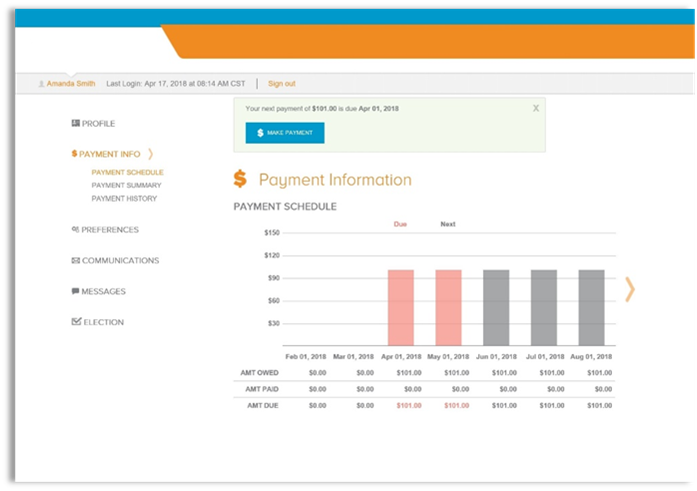
Online Payments
Ready to Get Started?
What exactly is COBRA?
COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Both full- and part-time employees are counted to determine whether a plan is subject to COBRA. Each part-time employee counts as a fraction of a full-time employee, with the fraction equal to the number of hours worked divided by the hours an employee must work to be considered full time. For example, if full-time employees at Company A work 40 hours per week, a part-time employee who works 20 hours per week counts as half of a full-time employee, and a part-time worker who works 16 hours per week counts as four-tenths of a full-time employee.
What Events qualify for COBRA?
-
Voluntary termination
-
Involuntary termination
-
Reduction of employee hours
-
Death of employee
-
Divorce or legal separation
-
Medicare entitlement (in extremely rare circumstances)
-
Dependent child ceasing to be a dependent
What coverages are
Eligible for COBRA
-
Medical
-
Prescription
-
Dental
-
Vision
-
Health FSA
-
HRA
-
Certain EAPs
What Events qualify for COBRA?
-
Voluntary termination
-
Involuntary termination
-
Reduction of employee hours
-
Death of employee
-
Divorce or legal separation
-
Medicare entitlement (in extremely rare circumstances)
-
Dependent child ceasing to be a dependent
What coverages are
Eligible for COBRA
-
Medical
-
Prescription
-
Dental
-
Vision
-
Health FSA
-
HRA
-
Certain EAPs
What exactly is COBRA?
COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Both full- and part-time employees are counted to determine whether a plan is subject to COBRA. Each part-time employee counts as a fraction of a full-time employee, with the fraction equal to the number of hours worked divided by the hours an employee must work to be considered full time. For example, if full-time employees at Company A work 40 hours per week, a part-time employee who works 20 hours per week counts as half of a full-time employee, and a part-time worker who works 16 hours per week counts as four-tenths of a full-time employee.

Non-Compliance can be expensive.
The IRS and DOL can levy fines and taxes for noncompliance with COBRA, including excise taxes for each qualified beneficiary impacted by a failure during a compliance period. Employers may also face penalties under the Employee Retirement Income Security Act (ERISA).
Possible Additional Costs:
Insurance carriers can recover claim payments for anyone that was offered COBRA over their allowed date.
You could be obligated to cover medical expenses if you can't prove you offered COBRA within the mandatory COBRA timeframe.
The employer can be held liable for payment of legal fees and court costs.
$100 per day for each qualified beneficiary (excise tax)
$110 per day under ERISA
We will gather the required information to set up your plan(s) and identify any members that need to transition.
Initial Set Up
We manage COBRA timelines to ensure all regulation language is included in all required communications. State continuation options available.
Compliance
We will ensure members receive timely communication including all COBRA required notices, payment coupons, monthly statements, open enrollment notices, and more. Online or paper enrollment options are available.
Communication
All communication is sent with COBRA regulation, bar coded, and all mailed letters time/date stamped, using the industry’s only “postmark date aware” lockbox.
Fulfillment
We collect the premium due and provide accurate administration including remittance and account reports. Electronic and paper check payments allowed.
Premium Collection & Remittance
We will automatically track when a COBRA member should be terminated due to non-payment or end of coverage period and issue the required notices.
Termination/End of COBRA
Modify plan setup including the ability to support many complete plan and rate structures and issue rate change notifications.
Renewal Processing
We provide full transparency into enrollments/payments in a variety of formats. Reports are available OnDemand or can be scheduled via the Employer Portal.
Reporting
Flexibility to accommodate numerous direct billing scenarios including COBRA, Leave of Absence (LOA), Long Term Disability (LTD), Retiree, Pet Insurance, State Continuation, and many others.
Direct Billing Options
Let us Take Care Of Everything

MoneyWise also offers additional Year Round Compliance Solutions!
Explore our Compliance Packages tailored for businesses of every scale. Take a look!
Helpful Links
View all Participant Info, Run Reports, View Payments
View all Groups and Participant Info, Run Reports, View Payments
Enroll, Make Payment, Review Documents
View and Download helpful Materials
COBRA Frequently Asked Questions
COBRA – the Consolidated Omnibus Budget Reconciliation Act -- provides a temporary continuation of group health coverage that would otherwise be lost due to certain life events.
A group health plan must offer COBRA continuation coverage only to qualified beneficiaries and only after a qualifying event has occurred.
A qualified beneficiary is an employee who was covered by a group health plan on the day before a qualifying event occurred, or it could also be an employee's spouse, former spouse, or dependent child who was on the plan the day before the qualifying event occurred.
Qualifying events are events that cause an individual to lose group health coverage. The type of qualifying event determines who the qualified beneficiaries are and the period of time that a plan must offer continuation coverage. COBRA establishes only the minimum requirements for continuation coverage. A plan may always choose to provide longer periods of continuation coverage and/or contribute toward the cost. The following are qualifying events for a covered employee if they cause the covered employee to lose coverage:
-
Termination of the covered employee’s employment for any reason other than “gross misconduct,” or
-
Reduction in the covered employee’s hours of employment
The following are qualifying events for a spouse and dependent child of a covered employee if they cause the spouse or dependent child to lose coverage:
-
Termination of the covered employee's employment for any reason other than “gross misconduct,”
-
Reduction in hours worked by the covered employee,
-
Covered employee becomes entitled to Medicare,
-
Divorce or legal separation from the covered employee, or
-
Death of the covered employee.
In addition to the above, the following is a qualifying event for a dependent child of a covered employee if it causes the child to lose coverage:
-
Loss of “dependent child” status under the plan rules. Under the Affordable Care Act, plans that offer coverage to children on their parents’ plan must make coverage available until the child reaches the age of 26.
-
Group health plans can require qualified beneficiaries to pay for COBRA continuation coverage, although plans can choose to provide continuation coverage at reduced or no cost. The maximum amount charged to qualified beneficiaries cannot exceed 102 percent of the cost to the plan for similarly situated individuals covered under the plan who have not incurred a qualifying event.
In calculating premiums for continuation coverage, a plan can include the costs paid by both the employee and the employer, plus an additional 2 percent for administrative costs. For qualified beneficiaries receiving the 11-month disability extension of continuation coverage, the premium for those additional months may be increased to 150 percent of the plan's total cost of coverage. Plans may increase COBRA premiums for qualified beneficiaries if the cost to the plan increases, but generally plans must fix premiums before each 12-month premium cycle.
The plan must allow qualified beneficiaries to pay the required premiums on a monthly basis if they ask to do so, and may allow payments at other intervals (for example, weekly or quarterly). Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election. Plans must provide at least 45 days after the election (that is, the date the qualified beneficiary mails the election form if using first-class mail) for making an initial premium payment. If a qualified beneficiary fails to make any payment before the end of the initial 45-day period, the plan can terminate the qualified beneficiary’s COBRA rights.
The plan should establish due dates for any premiums for subsequent periods of coverage, but it must provide a minimum 30-day grace period for each payment. Plans can terminate continuation coverage if full payment is not received before the end of a grace period. If the amount of a payment made to the plan is incorrect, but is not significantly less than the amount due, the plan must notify the qualified beneficiary of the deficiency and grant a reasonable period (for this purpose, 30 days is considered reasonable) to pay the difference. The plan is not obligated to send monthly premium notices, but must provide a notice of early termination if it terminates continuation coverage early due to failure to make a timely payment.
Please contact MoneyWise Solutions at help@moneywisesolutions.com or call 888-994-9392
If the group plan requires loss of coverage due to Medicare Eligibility, it may be a COBRA Qualifying Event. However, if an actively enrolled participant CHOOSES to drop the group plan because they have age qualified for Medicare, their Dependents are NOT guaranteed COBRA Rights. If this occurs, written approval must be received from the carrier(s).

COBRA & Direct Billing Member App
Managing your COBRA Elections just got easier.
Stay up to date and worry free with the MoneyWise COBRA & Direct Billing App! Manage your plans 24/7 through the intuitive design and navigation while on the go. Powerful features of this app include:
-
Plan Information
-
Payments made to your benefits
-
View notifications and receive messages
COBRA & Direct Billing Member App
Managing your COBRA Elections just got easier.
Stay up to date and worry free with the MoneyWise COBRA & Direct Billing App! Manage your plans 24/7 through the intuitive design and navigation while on the go. Powerful features of this app include:
-
Plan Information
-
Payments made to your benefits
-
View notifications and receive messages


Non-Compliance can be expensive.
The IRS and DOL can levy fines and taxes for noncompliance with COBRA, including excise taxes for each qualified beneficiary impacted by a failure during a compliance period. Employers may also face penalties under the Employee Retirement Income Security Act (ERISA).
Possible Additional Costs:
-
Insurance carriers can recover claim payments for anyone that was offered COBRA over their allowed date.
-
You could be obligated to cover medical expenses if you can't prove you offered COBRA within the mandatory COBRA timeframe.
-
The employer can be held liable for payment of legal fees and court costs.
$100 per day for each qualified beneficiary (excise tax)
$110 per day under ERISA
We will gather the required information to set up your plan(s) and identify any members that need to transition.
Initial Set Up
We manage COBRA timelines to ensure all regulation language is included in all required communications. State continuation options available.
Compliance
We will ensure members receive timely communication including all COBRA required notices, payment coupons, monthly statements, open enrollment notices, and more. Online or paper enrollment options are available.
Communication
All communication is sent with COBRA regulation, bar coded, and all mailed letters time/date stamped, using the industry’s only “postmark date aware” lockbox.
Fulfillment
We collect the premium due and provide accurate administration including remittance and account reports. Electronic and paper check payments allowed.
Premium Collection & Remittance
We will automatically track when a COBRA member should be terminated due to non-payment or end of coverage period and issue the required notices.
Termination/End of COBRA
Modify plan setup including the ability to support many complete plan and rate structures and issue rate change notifications.
Renewal Processing
We provide full transparency into enrollments/payments in a variety of formats. Reports are available OnDemand or can be scheduled via the Employer Portal.
Reporting
Flexibility to accommodate numerous direct billing scenarios including COBRA, Leave of Absence (LOA), Long Term Disability (LTD), Retiree, Pet Insurance, State Continuation, and many others.
Direct Billing Options
Let us Take Care Of Everything
COBRA Frequently Asked Questions
COBRA – the Consolidated Omnibus Budget Reconciliation Act -- provides a temporary continuation of group health coverage that would otherwise be lost due to certain life events.
A group health plan must offer COBRA continuation coverage only to qualified beneficiaries and only after a qualifying event has occurred.
A qualified beneficiary is an employee who was covered by a group health plan on the day before a qualifying event occurred, or it could also be an employee's spouse, former spouse, or dependent child who was on the plan the day before the qualifying event occurred.
Qualifying events are events that cause an individual to lose group health coverage. The type of qualifying event determines who the qualified beneficiaries are and the period of time that a plan must offer continuation coverage. COBRA establishes only the minimum requirements for continuation coverage. A plan may always choose to provide longer periods of continuation coverage and/or contribute toward the cost. The following are qualifying events for a covered employee if they cause the covered employee to lose coverage:
-
Termination of the covered employee’s employment for any reason other than “gross misconduct,” or
-
Reduction in the covered employee’s hours of employment
The following are qualifying events for a spouse and dependent child of a covered employee if they cause the spouse or dependent child to lose coverage:
-
Termination of the covered employee's employment for any reason other than “gross misconduct,”
-
Reduction in hours worked by the covered employee,
-
Covered employee becomes entitled to Medicare,
-
Divorce or legal separation from the covered employee, or
-
Death of the covered employee.
In addition to the above, the following is a qualifying event for a dependent child of a covered employee if it causes the child to lose coverage:
-
Loss of “dependent child” status under the plan rules. Under the Affordable Care Act, plans that offer coverage to children on their parents’ plan must make coverage available until the child reaches the age of 26.
-
Group health plans can require qualified beneficiaries to pay for COBRA continuation coverage, although plans can choose to provide continuation coverage at reduced or no cost. The maximum amount charged to qualified beneficiaries cannot exceed 102 percent of the cost to the plan for similarly situated individuals covered under the plan who have not incurred a qualifying event.
In calculating premiums for continuation coverage, a plan can include the costs paid by both the employee and the employer, plus an additional 2 percent for administrative costs. For qualified beneficiaries receiving the 11-month disability extension of continuation coverage, the premium for those additional months may be increased to 150 percent of the plan's total cost of coverage. Plans may increase COBRA premiums for qualified beneficiaries if the cost to the plan increases, but generally plans must fix premiums before each 12-month premium cycle.
The plan must allow qualified beneficiaries to pay the required premiums on a monthly basis if they ask to do so, and may allow payments at other intervals (for example, weekly or quarterly). Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election. Plans must provide at least 45 days after the election (that is, the date the qualified beneficiary mails the election form if using first-class mail) for making an initial premium payment. If a qualified beneficiary fails to make any payment before the end of the initial 45-day period, the plan can terminate the qualified beneficiary’s COBRA rights.
The plan should establish due dates for any premiums for subsequent periods of coverage, but it must provide a minimum 30-day grace period for each payment. Plans can terminate continuation coverage if full payment is not received before the end of a grace period. If the amount of a payment made to the plan is incorrect, but is not significantly less than the amount due, the plan must notify the qualified beneficiary of the deficiency and grant a reasonable period (for this purpose, 30 days is considered reasonable) to pay the difference. The plan is not obligated to send monthly premium notices, but must provide a notice of early termination if it terminates continuation coverage early due to failure to make a timely payment.
Please contact MoneyWise Solutions at help@moneywisesolutions.com or call 888-994-9392
If the group plan requires loss of coverage due to Medicare Eligibility, it may be a COBRA Qualifying Event. However, if an actively enrolled participant CHOOSES to drop the group plan because they have age qualified for Medicare, their Dependents are NOT guaranteed COBRA Rights. If this occurs, written approval must be received from the carrier(s).

Helpful Links
View all Participant Info, Run Reports, View Payments
View all Groups and Participant Info, Run Reports, View Payments
Enroll, Make Payment, Review Documents
View and Download helpful Materials